
Category: Social Issue


Climate Change, Migration and Healthcare in Gonaives

A tale of two Haiti(s)

Why Haitian Doctors Choose To Practice In Haiti

On the shades of violence in Haiti

The weight of social approval

Let’s change the rules to save women’s lives in Haiti
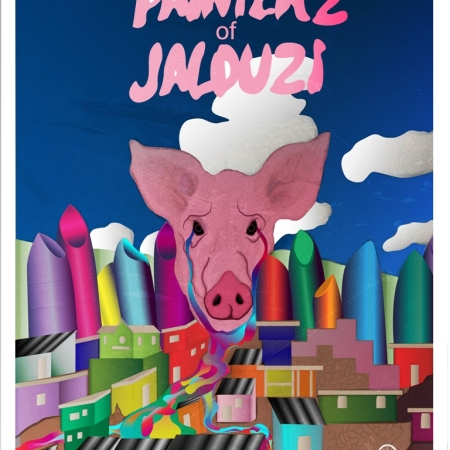
Beneath the Beautiful Bright Paint Covering Jalouzi
